What is NIPT and what was it developed for?
Until some years ago, the sex of an unborn baby could only be predicted as early as the second trimester of pregnancy, so between weeks 13 and 27, by the means of an ultrasound. In 2011 Noninvasive Prenatal Genetic Testing (NIPT) has been introduced to clinical practice [2]. NIPT has revolutionized prenatal care by offering expecting couples a reliable, accurate and noninvasive (it only requires a blood sample from the expecting mother) procedure to predict a multitude of genetic disorders and features of the fetus.
The NIPT era began with the discovery of about 10% cell-free fetal DNA/RNA (cffD-NA/RNA) in maternal plasma in 1997 [3]. These DNA fragments can be detected as early as week seven of gestation. They originate directly from the placenta and they clear out in the first day after delivery. Therefore, they are ideal to look for genetic traits of the fetus, requiring just a blood sample of the mother, while being sure that the DNA examined does not represent remainings of past pregnancies.
The initial use of the test was to look for trisomies (i.e. genetic disorders in which a person has three copies of a particular chromosome instead of the normal two copies), such as Down Syndrome, Patau Syndrome or Edwards Syndrome. These disorders cause severe intellectual and physical disabilities, so an early diagnosis can make a big difference in the life of the expecting parents and their child.
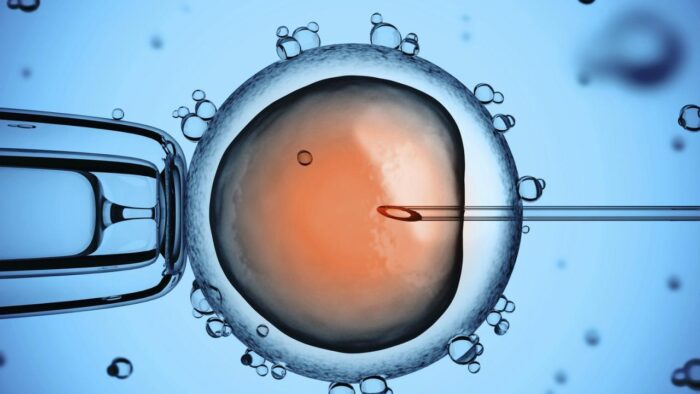
Before NIPT, the only way to diagnose trisomies before birth was via invasive procedures such as Chorionic villus sampling (CVS) or amniocentesis. Both involve introducing a needle directly into the pregnant women's womb and taking out a small sample of placental tissue or amniotic fluid. The problem with this procedure is the miscarriage risk. Earlier studies from 2006 [4] and 2009 [5] report 1 - 2% miscarriage risk (so about 1 in 100 women undergoing the procedure). More recent studies, like the one from 2014 by Akolekar et al. [6], report significantly lower miscarriage risks of 0.11 - 0.22 %. Even though the risk seems small, when taking into account the number of women undergoing the procedure, it could still mean that about 350 babies are lost each year (if the risk is assumed to be 1%), some of which were actually not affected by any genetic disease [7]. Regardless of only a small risk involved, miscarrying a wanted baby is still a scary thought to many pregnant women, who would rather try everything else before undergoing CSV or amniocetesis.
Here is where NIPT comes into play. With a sensitivity of 95% (i.e. the probability that the test will detect a trisomy), a specificity of 99% (i.e. the probability that the test will correctly identify blood samples without a trisomy) and a known prevalence value (i.e. how often the disease occurs in the populations), the test is an accurate method of ruling out trisomies [8]. Nevertheless, NIPT is not yet considered a diagnostic test, but merely a screening method. That means, should the test results come out positive, an invasive procedure is still required for confirmation. Still, by first using NIPT, the number of women undergoing invasive tests is significantly reduced. Only the women who test positive in NIPT are directed to CVS or amniocentesis, thus further reducing the miscarriage risk of healthy fetuses.
So far, NIPT might seem like a harmless and highly useful test for any pregnant woman at risk of carrying a fetus with a chromosomal abnormality. But there are many ethical questions concerning NIPT. One of the discussion points being: could NIPT increase the number of sex-selective abortions?
Missing Girls
In countries like China or India, there is a long history of female infanticide (killing baby girls right after birth). The reasons are ranging from a cultural preference of sons, to poverty and the dowry system, which makes girls seem a financial burden on the family. With the progress of medicine, the term "gendercide" (killing members of a specific gender systematically) has also come to include sex-selective abortions. These practices have resulted in skewed male-to-female ratios, for example 125 boys to 100 girls in China (reported in year 2000) and 126 boys to 100 girls in some states of India [1]. To put these numbers in perspective: the normal male-to-female ratio is about 104 boys to 100 girls. The long-term implications of these artificial demographic manipulations could be devastating for the society, if no actions to stop these practices are being taken.
This poses a difficult problem from an ethical as well as from a social perspective for NIPT testing. Since the karyotype is examined within the NIPT test, finding out whether the fetus has two X chromosomes, or an X and a Y is quite straight forward. The result: parents undergoing NIPT could find out the sex of their baby earlier than ever before. Does NIPT thus further increase the gender imbalance in the countries already affected by the phenomenon of gendercide? Trying to tackle this problem leads us to the following two questions:
1. What measures can/have already been taken to make sure NIPT does not increase the sex-selective abortions?
2. What steps can be made to stop gendercide, especially directed to girls?
Towards the goal of stopping gendercide
Since the introduction of NIPT to clinical practice, some laws have been enacted and ethical "best practices" have been formulated in order to prohibit and discourage sex-selective abortions in the European Union (EU) and the United States of America (USA). Even though countries from EU and the USA are generally not the ones where gendercide has been reported and directly proven, these measures are important so that they do not become centers for sex-selective abortion tourism. The genetic data protection in the EU is guaranteed by the "Regulation (EU) 2016/679 of the EU and the Council" from 27 April 2016 and by the "Directive (EU) 201/680 of the European Parliament and of the Council" from 27 April 2016. Many recommendations and guidelines on the use of non-invasive prenatal tests are given in [9]. Amongst others, the article advises offering testing only through licensed clinicians and not directly to consumers. Implementing this recommendation could lead to avoiding routinization of the tests, in cases where the determination of the sex is not needed (for example, if no risk of sex chromosome aneuploidies, i.e. abnormalities in the sex chromosomes X or Y, is detected) [10].
In some countries, such as the Netherlands, data regarding the gender of the fetus is not collected. Other countries, such as Switzerland, are debating passing a law that would only allow disclosing the gender of the fetus after the 12th week of pregnancy [11]. Even the countries with a long history of sex-selection abortions and gendercide, China and India, have passed laws that make these practices illegal. In China, sex selections for non-medical reasons are prohibited for more than twenty years [12]. In India, the law of Prenatal Diagnostic Techniques (Regulation and Prevention of Misuse) Act 5 prohibits use of prenatal diagnostic techniques and tests to acquire information on fetal sex [10].
However, with the growing number of NIPTs carried out in China and India (twice the number of test carried out in the USA and 33 times that in Europe [10]), more research and monitoring is necessary in these countries to ensure that the companies and hospitals offering NIPT are actually obeying the law.
It is worthwhile to recall, however, that gendercide is not only caused by abortions, but also through female infanticide. Though these obviously illegal and cruel murdering of healthy newborns might seem like a thing of the past, there are numerous evidences that they are still continuing in poor regions of developing countries. The 2012 documentary "It's a Girl: The Three Deadliest Words in the World" directed by Evan Grae Davis brings the femicide happening mostly in China and India into the spotlight. The documentary reports disturbing United Nations (UN) data revealing that almost 200 million girls are missing in the world because of gendercide. And even though the dowry system in India has been banned for decades, the tradition is far away from being forgotten, lowering the status of women and endangering girls coming from a poor family. Therefore, beside making sure that sex determination of fetuses is hindered, great efforts should also be made into raising the social status of women in the countries where gendercide is still a reality. This includes access to education to all women and enabling them to find jobs and become independent, so that they stop being seen as a financial burden by the family. This is definitely a difficult and long-lasting process in countries with a long tradition of male dominance. Nonetheless, it is the responsibility of us living in economically rich countries to not only create and provide equal access to new medical screening tests in developing countries, but also make sure those tests are accompanied by proper counselling adapted to the moral and traditional values of the patients.
References
Seema Mohapatra. Global legal responses to prenatal gender identification and sex selection. Nevada Law Journal, 13(3, article 5), 2013. http://scholars.law.unlv.edu/nlj/vol13/iss3/5.
Allyse M, Minear MA, Berson E, and et al. Non-invasive prenatal testing: a review of international implementation and challenges. International Journal of Womens Health, 7:113{126, 2015.
ADe Jong A, Dondorp WJ, de Die-Smulders CEM, Frints SGM, and deWert GMWR. Non-invasive prenatal testing: ethical issues explored. European Journal of Human Genetic, 18(3):272{277, 2010.
Aaron B Caughey, Linda M Hopkins, and Mary E Norton. Chorionic villus sampling compared with amniocentesis and the difference in the rate of pregnancy loss. Obstetrics & Gynecology, 108(3):612{616, 2006.
A Tabor, CHF Vestergaard, and O Lidegaard. Fetal loss rate after chorionic villus sampling and amniocentesis: an 11-year national registry study. Ultrasound in obstetrics and gynecology, 34(1):19{24, 2009.
R Akolekar, J Beta, G Picciarelli, C Ogilvie, and F d'Antonio. Procedure-related risk of miscarriage following amniocentesis and chorionic villus sampling: a systematic review and meta-analysis. Ultrasound in Obstetrics & Gynecology, 45(1):16{26, 2015.
Sarah Knapton. Hundreds of babies could be saved after down's syndrome blood test is approved for NHS, Access date: 09.06.2018. Website: Telegraph.co.uk https://www.telegraph.co.uk.
Shantanu Rane. To NIPT or not to NIPT?, Access date: 09.06.2018. Website: Medium https://medium.com.
Allyse M, Sayres L, Havard M, and et al. Best ethical practices for clinicians and laboratories in the provision of non-invasive prenatal testing. Prenatal diagnosis, 33(7):656{661, 2013.
Narine Harutyunyan. Non-invasive prenatal testing: a new tool for sex selections? University of Bologna, 2017. https://www.dilemata.net.
Bundesamt BAG. Revision Gesetz über genetische Untersuchungen beim Menschen, Access date: 04.07.2018. Website: Bag.admin.ch https://www.bag.admin.ch.
Npc.gov.cn. Law of the people's republic of china on maternal and infant health care, Access date: 09.06.2018. http://www.npc.gov.cn.
Die Beiträge auf dem Reatch-Blog geben die persönliche Meinung der Autor*innen wieder und entsprechen nicht zwingend derjenigen von Reatch oder seiner Mitglieder.

Comments (0)